AbilTo, a health IT startup that focuses on helping people with chronic conditions change how they psychologically manage their health, has raised a $12 million Series C round, the company said.
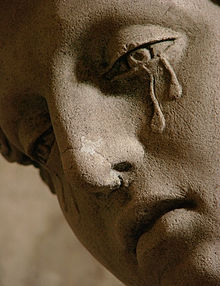
The company works with health plans by offering members eight-week programs to improve recovery by teaching people to better cope with stress and sadness through interactive videos or phone conversations. It aims its services at people with heart conditions, Type 2 diabetes, postpartum depression, breast cancer and pain-management issues, among other problems.
“Participants meet with a clinical social worker and behavior coach separately, once a week, either by phone or in a Web-based video chat,” MedCity News reported.