This fascinating interview in ConvergenceRI with Louis Giancola, the CEO of South County Health, whose South County Hospital is Rhode Island’s remaining independent acute-care hospital, gives a very interesting overview of the challenges facing such institutions.
Among other things, he talked with the news service’s editor, Richard Asinof, about how, in Mr. Asinof’s words, “the new models of Accountable Care Organizations and accountable entities with managed Medicaid programs were being developed in Rhode Island” in the new age of population health.
Mr. Giancola worried about how the state’s population was going to be divided up:
“There are a million people in Rhode Island, and you’re going to carve the population up by ACOs, which is not consistent with communities, not geographically. It will be payer- specific, and it is going to cut across a lot of different communities.”
The Department of Health and Human Services touted a new study published in the New England Journal of Medicine as evidence that the Affordable Care Act (ACA) has cut preventable readmissions.
HHS researchers analyzed data from 3,387 hospitals and found readmission rates have fallen sharply since the ACA’s implementation, particularly for conditions that carry readmission penalties under the ACA. Readmission rates dropped to 17.8 percent from 21.5 percent from 2007 to 2015, according to the findings.
Although the study also found an increase in observation status, researchers noted the trend began in 2008, two years before the passage of the ACA. Researchers also found that while “preventable readmissions” have declined, so, too, have overall returns to the hospital within 30 days of discharge — a broader measure that encompasses observation stays and readmissions.
“Readmission trends are consistent with hospitals’ responding to incentives to reduce readmissions, including the financial penalties for readmissions under the ACA,” the authors wrote. “We did not find evidence that changes in observation-unit stays accounted for the decrease in readmissions.”
In an HHS blog post, Rachael Zuckerman, an economist with the HHS Office of the Assistant Secretary for Planning and Evaluation, said the research vindicated the readmissions program in the face of the allegations of deceptive hospital practices. She said that “the Hospital Readmissions Reduction Program is just one part of the administration’s broader strategy to promote better care, smarter spending and healthier people by paying providers for what works, unlocking healthcare data, and finding new ways to coordinate and integrate care to improve quality” through such improvements as Accountable Care Organizations.
The Centers for Medicare & Medicaid Services (CMS) and America’s Health Insurance Plans (AHIP), the main private-health-insurance lobbying group, have unveiled new sets of core measures for quality care.
The Core Quality Measures is a collaboration to design and implement a standard set of metrics across payers so that providers who have been forced to report different quality metrics on a payer-by-payer basis get their administrative burdens reduced as CMS and private payers move to a common system.
The seven new measure sets include metrics for Accountable Care Organizations/patient-centered medical homes, primary-care cardiology, gastroenterology, HIV/hepatitis C, medical oncology, orthopedics, obstetrics and gynecology.
The announcement is a step in the transition from the traditional fee-for-service model. Fierce HealthPayer noted: “While improved quality of care provides an attractive philosophical underpinning for a value-based care model, it’s very difficult for practices to take pragmatic steps toward improving their quality of care without knowing how payers define quality and, more importantly, how they intend to measure it.”
This New England Journal of Medicine article looks at how to address the problems of the high-risk patients in Accountable Care Organizations.
“Since a small percentage of patients account for the majority of health care spending, high-risk- care management could substantially reduce costs and improve quality. But heterogeneity in clinical needs complicates efforts to develop integrated strategies.”
This piece looks at what it takes to be a strong physician leader in an age increasingly focused on population health. The authors, Kathy Jordan, president of Jordan Search Consultants, and Regina Levison, Jordan Search’s vice president of client development, conclude:
“In the era of population health management, the need for competent physician leaders will increase exponentially. Not only will primary care physicians (PCPs) direct care management teams to manage patient populations, but advanced practice providers, nurses, social workers, pharmacists and other non-clinical workers will also be required to lead teams and colleagues. The new paradigm necessitates it, but the statistics for best practices support it. According to a white paper published by the American Association for Physician Leadership, there is a link between physician leadership and organizational success; 21 of the 29 pioneer Accountable Care Organizations that earned bonuses from the Centers for Medicare and Medicaid Services were organizations led by physicians.
Effective clinical leaders will be the determining factor for success and growth in this new healthcare environment; as such, it is imperative that physicians are well-equipped to lead and organizations are prepared to better evaluate effective leaders. The competent, effectual physician leader appropriately employed by a strategic, visionary organization will create the dynamic needed to successfully navigate this new era of healthcare and improve the health of populations nationwide.”
Healthcare research and policy consultant David Introcaso argues in a HealthAffairs post that Medicare Advantage plans should be included in the federal government’s goal to transition Medicare to a value-based payment system.
Part of the explanation for MA plans’ exclusion so far might be that the Centers for Medicare and Medicaid Services doesn’t know enough about how MA plans reward physicians for quality and value.
In any event, he says, excluding MA plans from the government’s goal ignores “substantial and rapidly growing” MA spending. Mr. Introcaso notes that MA is expected to have more than 25 million enrollees by 2024, meaning that about 30 percent of all Medicare payments would be left out of the government’s value-based initiative if the regulations aren’t changed.
He argues for integrating alternative-payment models — especially Accountable Care Organizations (ACOs) — with MA plans, although that would require some major regulatory adjustments.
Donald S. Bialek, M.D., MPH, has joined Cambridge Management Group (CMG) as a senior adviser.
Dr. Bialek brings to Cambridge Management Group vast experience in care integration and healthcare informatics – two crucial elements of the current healthcare revolution. He helps physicians and hospitals redesign care, especially by modifying clinical workflow, to better manage value-based contracts for comprehensive care in Accountable Care Organizations and specific episodes in bundled-payment models.
His career shows a remarkable mix of streamlining and improving patient care in community settings and knowledge of new physician-practice models, including physician engagement with new information systems.
Dr. Bialek has served in a wide range of senior administrative, clinical leadership and consulting posts. He has worked with community hospitals, academic medical centers, physician groups, health-insurance plans and life-science companies in institutional governance, operational and strategic matters
His positions have included:
- Chairman, president and CEO of Alliance Medical Practices (primary-care-physician management).
- Chairman, president and CEO, Paradigm Medical Teams Inc. (hospital-based physician clinical contract management).
- Chairman, Aprus Inc. (physician-practice management and accounts-receivable management).
- Faculty, Harvard University.
- Director, Training & Education Group, International Health Systems Program, Department of Population and International Health, Harvard School of Public Health.
- Chairman, Department of Anesthesia and Critical Care, Quincy (Mass.) Hospital.
- Chairman of MIT’s Sloan School of Management seminar on “Aligning Information Technology and Business Strategy’’.
- Chief medical officer, Galloway Consulting.
- Managing director, Huron Consulting Group.
- Senior industry expert, Global Health Solutions, CSC Corp.
- Senior executive physician consultant, Dearborn Advisors.
Donald Bialek received a BSc. degree from the University of Maryland, a medical degree from the University of Minnesota and a master’s degree in public health from Harvard. He did residencies at Massachusetts General Hospital and Children’s Hospital in Boston and a fellowship at Children’s Hopsital in Boston. Dr. Bialek also completed advanced-management studies at Harvard Business School and a fellowship in medical informatics in the Harvard/MIT program.
Fierce Healthcare reports that a bipartisan group of U.S. senators has released a paper outlining policy initiatives “aimed at Medicare patients with multiple chronic diseases such as heart disease and diabetes” with the aim of improving treatment and controlling costs as payers and regulators continue the long slog toward emphasizing preventive care and pay-for-value to replace pay for episode-by-episode service.
The idea, of course, is to replace the traditional episode-by-episode approach with a population-health-based management system,
The proposals are divided into several categories, including, summarizes FierceHealthcare:
- “Patient and caregiver empowerment during the care delivery.
- “High-quality home care.
- “Expanding benefit innovation and technology access.
- “Expanding interdisciplinary, team-based care access.
- “Population-health management for chronically ill patients.
Fierce reports that “{s}pecific policy proposals include reducing care coordination barriers within Accountable Care Organizations (ACOs), extending hospice benefits to Medicare Advantage beneficiaries and expanding home-care models. The group also proposes giving Medicare Advantage and ACOs more flexibility to deliver essential non-health services for beneficiaries with multiple complex conditions.”
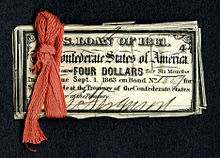
Where they make health policy in style.
“Faced with similar challenges and goals, as well as uncertainty about the best policy solutions, the United States and England have much to learn from each other in reforming health care. For example, the United States needs help in establishing policies that will encourage a primary care workforce that is as well developed and geographically distributed as the workforce in England. England also has much to learn from the experience in the United States of delivering population-based care management through Accountable Care Organizations. Ultimately, success in both countries will depend on, first, an unremitting focus on promoting collaboration among payers, physicians, organizations that provide health services, and the people who use health services and, second, a consistent commitment of policy makers to support rigorous, timely, and independent evaluations of health care policies.”