By RACHEL BLUTH
Kaiser Health News
A recent change in how Medicare pays for joint replacements is saving millions of dollars annually — and could save billions — without impacting patient care, a new study has found. But the man whom Donald Trump has picked to be the secretary of the Department of Health and Human Services has vocally opposed the new mandatory payment program and is likely to revoke it.
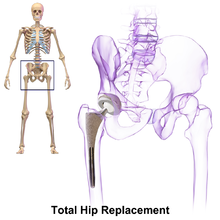
Under the new program, Medicare effectively agrees to pay hospitals a set fee — a bundled payment — for all care related to hip- or knee-replacement surgery, from the time of the surgery until 90 days after. Traditionally hospitals collect payments for many components of care and rehabilitation individually.
Tom Price, M.D., the president elect’s HHS nominee, a congressman from Georgia and a very affluent orthopedic surgeon, has actively opposed the idea of mandating bundled payments for these orthopedic operations, calling it “experimenting with Americans’ health,” in a letter to the Medicare agency just last September. In addition, the agency which designed and implemented the experiment, the Center for Medicare and Medicaid Innovation, was created by the Affordable Care Act to devise new methods for encouraging cost-effective care. It will disappear if the act is repealed, as President-elect Trump has promised to do.
The study appeared Jan. 3 in the Journal of the American Medical Association. Though one of its authors is Ezekiel Emanuel, M.D., a professor at the University of Pennsylvania who helped design the ACA, the research relies on Medicare claims data from 2008 through mid-2015, long before the presidential election.
Starting in April 2016, CMS required around 800 hospitals in 67 cities to use the bundled payment model for joint replacements and 90 days of care after the surgery as part of the Comprehensive Care for Joint Replacement program. The program had previously been road-tested on a smaller number of hospitals on a voluntary basis, which formed the focus of the research.
The study found that hospitals saved an average of 8 percent under the program, and some saved much more. Price has been skeptical that bundled payments did save money, but the researchers estimate that if every hospital used this model, it would save Medicare $2 billion annually.
The bundled payment program works like this: For some specific kinds of medical procedures, including joint replacements or some heart surgeries, the Centers for Medicare & Medicaid Services will add up the costs for the entire episode, from the hospital stay and medical supplies to the rehabilitation afterwards. If the total costs are below a target set by CMS, the hospital gets to keep the savings. If not, the hospital has to pay Medicare the difference. It’s supposed to incentivize more efficient spending and better care coordination between providers, so they can lower costs.
In practice, it seems to be working. Baptist Health System, a network of five hospitals in San Antonio, saved an average of $5,577 on each joint replacement without sacrificing the quality of care, according to the study. Baptist was an early adopter of bundled payments; it began experimenting with them in 2008. Over seven years, the hospital system has cut Medicare’s costs on knee replacements by almost 21 percent.
The savings came without impacting quality. Patients at Baptist Health System were just as likely to be readmitted to the hospital or end up in the emergency room as patients nationally. There was some indication that quality of care may be better, fewer patients under bundled payments had long, extended hospital stays.
In Price’s letter from September, he said that Medicare had exceeded its powers in imposing such bundled payments, which he said took decisions out of the hands of doctors and patients.
That doesn’t seem to be the case, according to Amol Navathe, M.D., an assistant professor of medicine and health policy at the University of Pennsylvania, and one of the authors of the JAMA study. Instead, Navathe and his colleagues suggest that the bundled payments actually fostered greater collaboration between surgeons, administrators and patients because programs could only succeed in saving money if physicians were engaged in creating standardized pathways for care.
For example, the Baptist Health System saved about 30 percent on implant costs, around $2,000 on each artificial joint, by using the least expensive medically equivalent implants as determined by the hospitals’ surgeons.
Usually, physicians are prevented from benefitting when hospitals save money because of anti-kickback laws. Waivers under bundled-payment models mean that surgeons can put in the time to find the best, most cost-effective implants, and share in some of that savings.
“It takes that extra level of effort and coordination, and proactively communicate with [patients],” Navathe said. “Preplanning, setting of expectations and communicating up-front is resource intensive, when they have the incentive to do that they were willing to expend the extra resources to make that happen.”
When bundles included care after a patient’s hospital stay, spending on rehabilitation went down 54 percent. That’s because hospitals took the time to match patients to the right level of care, Navathe said.
Patients who didn’t need to stay in a nursing home or rehab center were set up with home health care or physical therapy.
Price has objected to CMS making bundled payments mandatory, calling it an instance of federal overreach. But bundled payments only work if everyone has to participate, according to Darshak Sanghavi, M.D., the former director of prevention and population health at the Center for Medicare and Medicaid Innovation.
If hospitals can choose whether or not to participate, only the ones that are already delivering care efficiently –and coming in under CMS’s cost target — will use bundles and Medicare will constantly be paying out bonuses. The system needs to be mandatory, Sanghavi said, to pull in less efficient hospitals and give them incentive to change.
“Stopping the programs for ideological reasons I think impedes innovation in a way that is going to consign us to having really, really high costs of care that’s going to continue in the future,” Sanghavi said.
Bundled payments aren’t just for hip and knee replacements. On Dec. 20, CMS announced it would expand mandatory bundled payments to treatments for heart attacks, bypass surgery and cardiac rehab beginning in July 2017. In its waning days, the Obama administration is effectively throwing down the gauntlet to the incoming administration on bundled payments, one of its signature reforms.