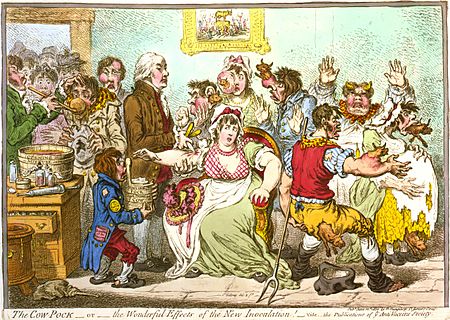
1802 caricature of Edward Jenner vaccinating patients who feared it would make them sprout cowlike appendages.
A new blueprint is needed to guide U.S. public health, focusing on food and housing security, good schools and transportation, as well as directly on medical care and illness and injury prevention, wrote Karen DeSalvo, acting assistant secretary for health at the Department of Health & Human Services, and Georges Benjamin, executive director of the American Public Health Association, in Health Affairs.
In other words, run American public health services more as governments do in the many other developed nations, in Western Europe and East Asia, that have far better health outcomes than does the U.S.
“Public Health 3.0” sees public health leaders as chief health strategists for their communities, in which there would be many cross-sector partnerships, including employers, insurers, education leaders and other stakeholders.
The blueprint would build on such earlier public health efforts as mass vaccinations, antibiotics, laboratory science, food and water safety and the professionalization and standardization of public health agencies.
“We must address the upstream drivers of health that touch everyone, no matter where they are born, live, learn, work, play, worship and age,” the authors wrote. “Public health is the essential infrastructure for this work, but it needs to innovate, and in many ways, reinvent itself so that we have what it takes to ensure that the American people are healthy, ready, and competitive in this global economy.”
Giving urgency to their proposals is that after decades of life expectancy growing in the U.S., average levels have been flat over the past three years and have actually dropped in some areas.
“Cross-sector partnerships to improve public health are already occurring across the country. ‘The traditional ‘silos’ of medical, behavioral and social services can’t meet the needs of our population alone,’’ Jim Hickman, CEO of Better Health East Bay, in California, told Healthcare Dive recently. “Partnerships, enabled by technology and amplified by data-sharing, are the first step in changing the way we deliver care.”
Other Public Health 3.0 blueprint steps include ensuring that all public health departments are nationally accredited, thus providing communities with “timely, reliable, granular-level … and actionable data,’’ establishing metrics to measure public health programs’ success and more flexible and sustainable funding sources.
To read the Health Affairs article, please hit this link.
To read a Healthcare Dive analysis, please hit this link.