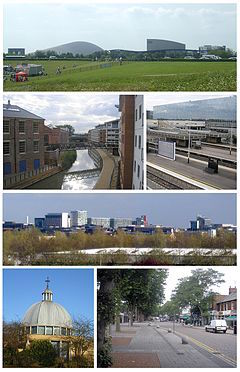
Scenes from Milton Keynes, in England.
The National Health Service in England may have some big lessons for the U.S. in adopting a value-based healthcare payment system, reports this HealthAffairs piece. Among the authors’ remarks:
“The first attempts at incentive change were relatively small scale. In 2011, payers in Milton Keynes… sought to improve substance misuse and sexual health services. They devised and developed a new form of contract to align financial incentives with system goals.
“The key elements of the new payment mechanism were that the contracts:
- “Were multi-year as opposed to annual.
- “Were based on capitation payments rather than fee for service.
- “Included outcome indicators that attracted annual additional payments of up to 20 percent for improved performance. Significantly the incentivized outcomes were identified through dialogue with people who used services.
“These capitated outcome-based and incentivized contracts (also known as COBIC) quickly resulted in better coordinated services, delivered at lower cost, and produced better outcomes.
“Since 2011, this initiative has been built upon and extended elsewhere. The next wave of outcomes-based COBICs addressed problems with services for single groups of disorders, most commonly musculoskeletal services …. As in the U.S., although not every initiative was successful, it was found that these contracts could quickly lead to better coordinated, more patient-centered care, with improved patient choice, good patient experience, and reduced costs.
“The concept is now being extended still further in both geography and ambition, with multi-year capitated outcomes-based COBICs being prepared and implemented for mental health care …, older people’s services …, and for people with long-term conditions…. One area, Somerset, has even begun to develop long-term per capita funded and outcomes-incentivized contracts for all the healthcare it buys for its whole population.
“The changes being catalyzed by these innovative approaches to payment are profound. They operationalize a value-based approach to healthcare, in which responsibility for population health is shared with providers. By placing more emphasis on achieving patient-defined outcomes, they make the whole system more patient-centric, shifting power from the providers to the people that use the system in terms not just of where and when services are provided, but what treatments and care an individual chooses to have in the first place.”
“The introduction of multi-year capitated outcome-incentivized contracts is a practical approach to operationalizing a value-based approach to care that can catalyze major change across a health economy at relative pace and scale (compared with the pace and scale of attempts at widespread transformation in the NHS’s recent past).”