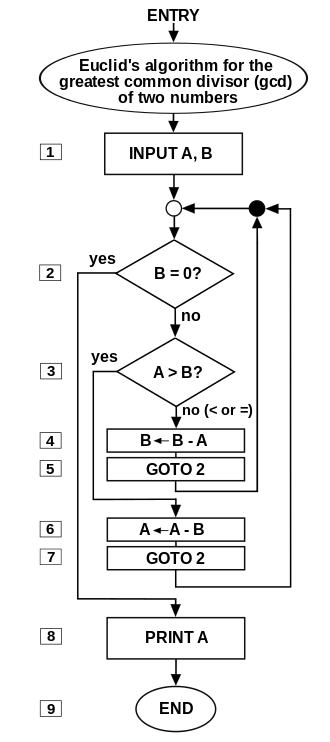
Flow chart of an algorithm.
Algorithms from machine learning have been beating humans in predicting such illnesses as heart disease and diabetes. Those algorithms will probably become even more accurate as they include personal data from smartphones and wearables, suggests an article from the Harvard Business Review.
Yannis Paschalidis, the director of the Center for Information Systems Engineering at Boston University, wrote in the Harvard Business Review that engineers at BU are working with such local hospitals as Brigham and Women’s Hospital and Boston Medical Center to manage heart disease and diabetes using algorithms that can predict hospitalizations up to a year in advance with 82 percent accuracy.
That’s compared, for example, to a 56 percent predictive accuracy of guidelines used by cardiologists to predict a patient’s risk of cardiovascular disease.
Of course, early identification of risk of serious diseases could save patients, providers and insurers billions of dollars as well a prevent many premature deaths.
Mr. Paschalidis, FierceHealthcare paraphrased, said that “machine learning will only become more accurate as data sets expand with access to personal data from wearables and smartphones. And as value-based payment models take hold, hospitals are likely to build analytics into their care processes.”
He wrote in the article: “If we can now predict future hospitalizations with more than 80% accuracy using medical records alone, imagine what is possible if we can tap into this trove of personal data. Recommender systems could be used to nudge us to adopt healthier eating habits and behaviors. The holy grail of heading off the emergence of conditions by keeping people well could be realized.”
Still, Mr. Paschalidis warned in his article:
“Yes, analytics and data-driven personalized medicine and health monitoring present risks. Do we want our employers and health insurers to know the status of our health and the risks we face? Privacy, security, and reliability of new systems and methods are also critical concerns. But rather than retreating from this new era, we should be working on how to strengthen our methods, institutions, laws, and regulatory framework to avoid those unintended consequences. Algorithms — the foundation of encryption methods, privacy-preserving data processing, and intrusion- and fraud detection systems — could help.”
T0 read the Harvard Business Review piece, please hit this link.
To read the FierceHealthcare report, please hit this link.