From FierceHealthcare:
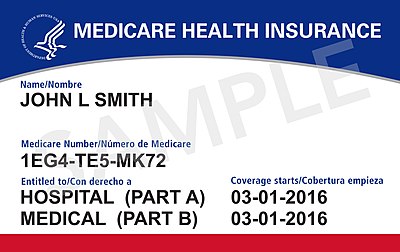
“Researchers examined changes in physician practice sizes associated with ACO market penetration three years after the launch of the Medicare Shared Savings Program, which began in 2012 and is one of the country’s largest ACO programs. In counties with more ACOs, they found more large practices and fewer small practices, according to a study published in Health Affairs.
“And they found evidence suggesting that ACO-driven physician consolidation is accelerating. ‘These patterns suggest that the consolidation concerns initially raised regarding ACOs were warranted and that gains from care coordination facilitated by ACOs will have to be balanced against higher prices and possibly lower-quality care that could result from consolidation,’ the study authors said.
“The catch is that while ACOs are associated with higher quality and lower costs, consolidation of physician practices is associated with lower quality and higher prices in some settings.”
To read the whole article, please hit this link.