Milton Packer asks in a Med Page Today piece if biomarkers will eventually replace physicians. He concludes:
“{I}F you are a non-procedural physician — someone who is paid to interact with patients, make a diagnosis, order tests, and prescribe non-procedural treatments — your days may be numbered. Artificial intelligence can easily do all of these things, with no need for an expensive intermediary.
“Artificial intelligence can even be programmed to say hello, ask about symptoms, and provide comforting words. The computer would be very thorough and can be programmed to be very empathetic. Arguably, some patients might not even notice the absence of a human presence, or miss it.
“Fortunately, that day has not yet arrived.
“However, if you are a physician who robotically moves through their daily routine with minimal patient interaction and with a heavy reliance on ordering and treating biomarkers, you are only one step away from making yourself obsolete. In ten years from now, who will need you?
“So here is my advice to all healthcare providers: The mission of delivering healthcare is being a healer — a uniquely human experience. If you do not want to be replaced by a computer, then you should stop acting as if you are following a programmed algorithm.
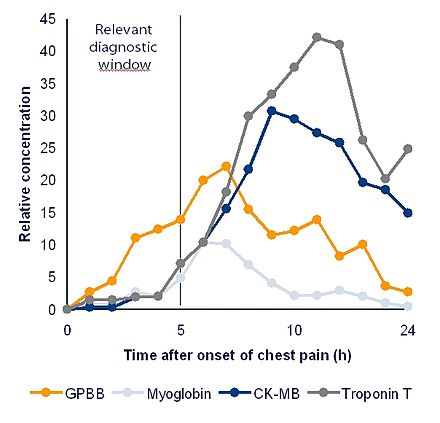
“Think about that the next time you order your next routine biomarker.”
To read his whole piece, please hit this link.