Jonathan Bush, athenahealth founder and CEO, writes here about how the future of the hospital is in the network.
He writes: “The vast majority of hospitals need to redefine themselves from organizations that deliver care to organizations that orchestrate care. Even though hospitals are one of the core lines of lifeblood in healthcare, the way in which the majority of them operate aren’t appealing to patients today, nor is it sustainable to hospitals’ future existence.”
“{O}ur {healthcare} system is so broken that it’s turned this instrument {the hospital} of health and humanity into a walled citadel. To better serve the patients who are seemingly already going elsewhere, hospitals need to become a leading orchestrator of the very best care on behalf of patients.”
The folks at New York-based Mount Sinai seem to get it. Last year, readers of The New York Times were treated to a Mount Sinai marketing campaign headline that read, ‘If our beds are filled, it means we’ve failed.’It’s counterintuitive, but spot on. Mount Sinai has embraced the idea that ‘instead of receiving care that’s isolated and intermittent, patients [should] receive care that’s continuous and coordinated, much of it outside of the traditional hospital setting.’ It’s only with this shift away from a ‘filling beds’ mindset, combined with a refactoring to the way in which a hospital interacts with other players in the market, that hospitals will maintain a leading role across the care continuum.”
He urges:
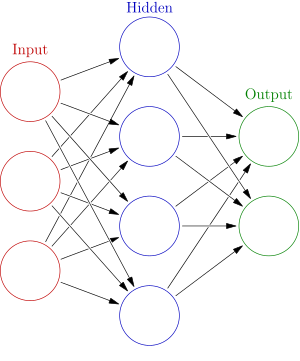
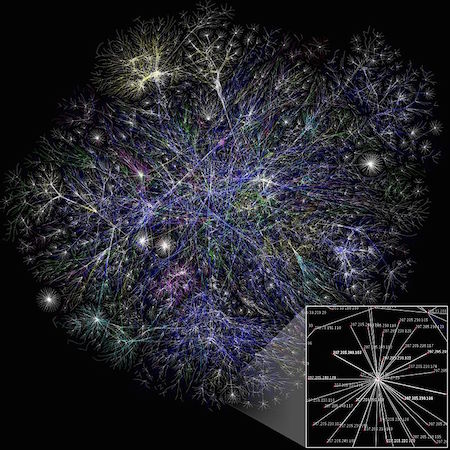
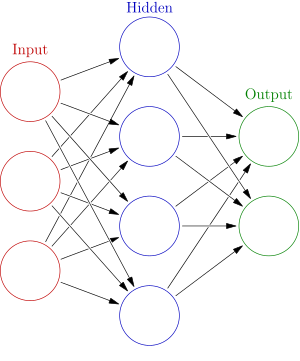
Embracing the “requirement to leverage an infrastructure of cross-continuum connectedness and total cost and quality transparency. Software alone won’t get hospitals there; being part of a more connected national network is critical.”
Adopting “savvier consumer marketing that helps hospitals stand out amidst emerging players in healthcare — like CVS Health and Walgreens — who understand the consumer mindset and have built their brands around convenience and ease.”
Accepting that a “new era of hospital sales must emerge, working with insurers and employers to broker deals that send the right patients through your doors only for the services you do really well.”
Realizing that “successful hospitals will create a renaissance of accessibility: If you can’t provide an appointment slot served up via a mobile app for every procedure type within three days, you’re failing.”
Understanding that “hospitals should become ecosystem partners, not brick-and-mortar investors. This means eliminating anything that can be done in a primary care practice, a retail clinic, or at home, and exporting non-invasive surgery out of the hospital to more cost-effective specialized surgical centers.”